More tips for managing diabetes while traveling around the world from Cazzy Magennis, of Dream Big Travel Far!
Planning ahead is crucial when traveling with diabetes. Though it may seem too challenging at first glance, traveling with type 1 diabetes can be done!
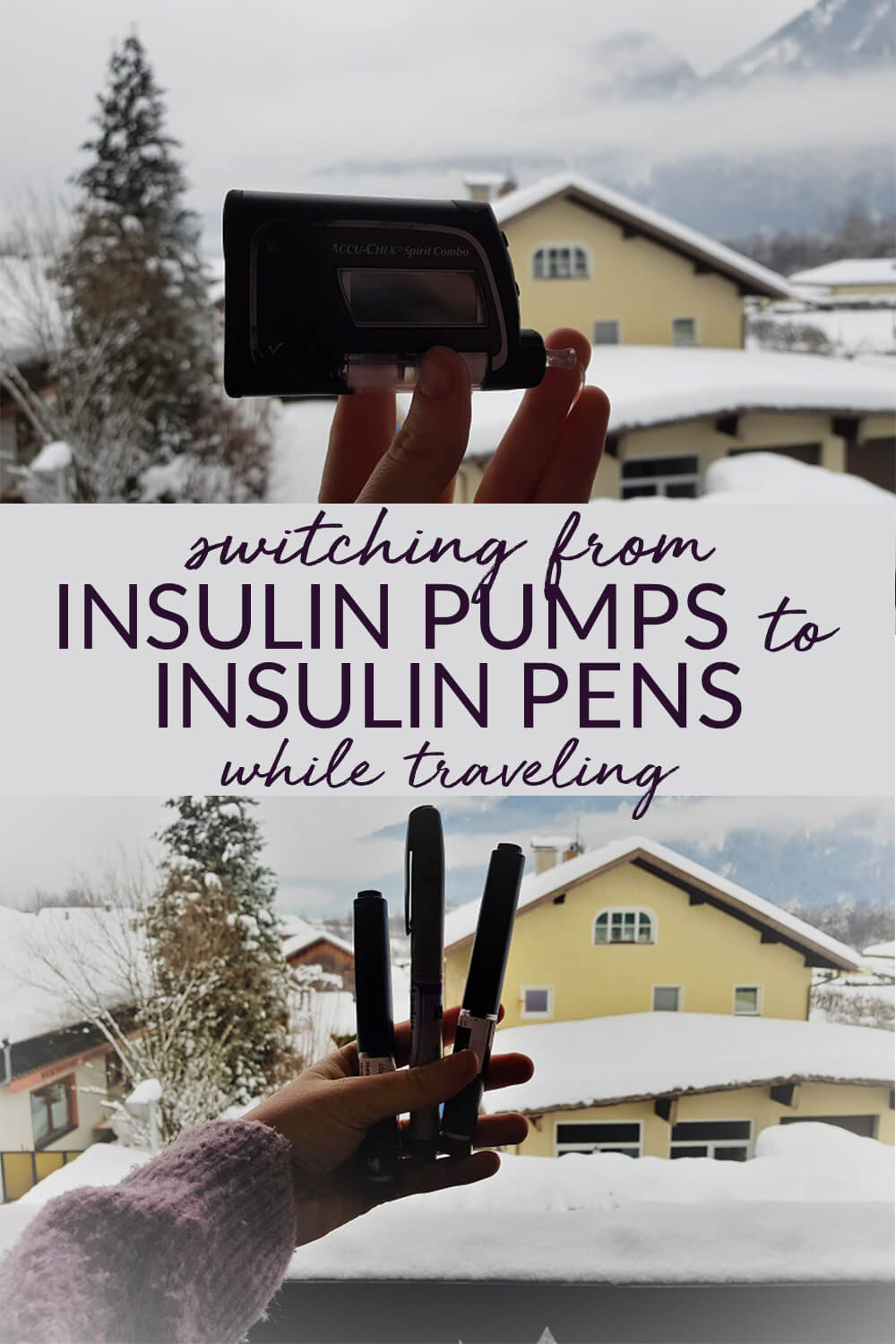
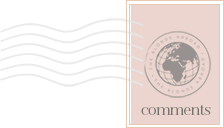
For any number of reasons, it may be necessary to switch from an insulin pump to an insulin pen while traveling. Whether you don’t want the inconvenience of pump sites or your trusty insulin pump breaks down, it’s always good to have a plan B.
To help, I’ve put together a guide on switching from insulin pumps to insulin pens while traveling.
When to Switch from an Insulin Pump to an Insulin Pen
Below are a number of scenarios, which some of you may not have considered, where you may need to make a temporary switch from an insulin pump to a pen:
- You’re spending the day submerged in water engaged in surfing, scuba diving, swimming, etc.
- Your insulin pump has been stolen or misplaced.
- Your insulin pump has died, and your replacement won’t arrive for a couple of days.
- Your insulin pump has died in the heat or cold, and you need to use pens temporarily.
- You’ve been admitted to the hospital, and the team won’t let you operate your pump.
There is one other important reason why you might want to make a temporary switch: you simply need a break.
Life with an insulin pump can feel demanding (and a bit frustrating, at times) because you are attached to something 24/7. There is absolutely no issue with wanting a break for a day or two!
Don’t feel like you can’t part with the pump for a bit. I’ve taken pump holidays before, and if anything, it makes me appreciate my insulin pump even more.

How to Make the Switch from Insulin Pens to Injections
The following advice is based on my own experience, and it may not work exactly the same way for you. With that said, it’s always best to seek advice from your doctor before you decide to take a break from your insulin pump.
Switch Duration: Less Than 24 Hours
- Every 3 – 4 hours, give yourself short-acting insulin.:
- Get the insulin you need for eating carbs and add correction doses as necessary. Remember that if you are doing any physical exercise, your blood sugar will decrease, so be mindful of your doses.
- Monitor frequently.
- When you’ve finished your activity, you can return to your insulin pump.
To keep from putting yourself at risk of a hypo, just remember that you need to wait 3-4 hours between injections, as you need to ensure all the insulin from the previous injection has left your body.
Switch Duration: 24 Hours
This is perfect for all those situations where an insulin pump is an inconvenience, such as on days spent at the beach, at a waterpark and so on.
For a one-day switch, you will typically only use your fast-acting insulin pen: Humalog. You will need to monitor your blood sugar much more frequently and give yourself fast-acting insulin every 3-4 hours (depending on the length of your insulin).
For example, if you’re surfing from 9 a.m. until sunset, don’t give yourself any background insulin, such as Lantus or Levemir. These can last up to 24 hours, which means you will need to wait until the background insulin has completely left your system before you can return to using an insulin pump.
Otherwise, you will have two sets of insulin in your body (your long-lasting insulin shot and your basal-rate insulin), which could put you at serious risk of multiple hypos.
Switch Duration: Greater Than 24 Hours
Regardless of why you switch for longer than 24 hours, your body is going to need long-lasting insulin and fast-acting insulin. There are two main ways to make this switch, with one being less tiresome than the other.
Option 1: Give yourself fast-acting insulin every 3-4 hours overnight, as you would during the day. The problem with this technique is that you need to wake up every 3-4 hours during the night, which isn’t exactly convenient.
However, if you don’t, your body will have absolutely no insulin going into it, which will put you at a high risk of diabetic ketoacidosis (DKA). So, it’s vital you only move forward with this option if you think you can commit to waking up. Of course, setting alarms will help you greatly!
Option 2: Give yourself a background dose of insulin in the form of either Lantus or Levemir and continue to bolus with your fast-acting insulin for meals and correction doses. This is the easier option, but your final dose of Lantus may be slightly different than your “total basal rate” that you take from your insulin pump.
Your insulin pump has been tailored to your body’s functions and is finely tuned, whereas Lantus isn’t as sensitive your body’s needs. So naturally, you may find you run slightly higher.
For a short-term period this isn’t much of an issue. You’ll know it’s working if your diet is low in carbs. If you’re running high, and you haven’t eaten any carbohydrates, then your dose likely isn’t high enough.
Be sure to take note of how your body has reacted for any further pump holidays you wish to take.
Chat with your doctor about the estimated dose of long-acting insulin you should take on a switch. They will know about your diabetic history, including details of the time before you started using a pump, so they’ll be able to suggest the best dosage for your needs.
Bonus Tips
- If you want to put your insulin pump back on early after a long-term switch, you should set your basal rate to 0.0 units per hour until all the Lantus or long-lasting insulin has left your body. You can bolus as necessary with your fast-acting insulin from your insulin pump.
- Monitor your numbers much more frequently than you normally would. It will be easier if you have a Freestyle Libre (which is now available in the USA!) or CGM system in place. However, these aren’t available for everyone, so more finger pricks will do the job just as well!
- Remember that your insulin requirements may change if you are engaging in physical activity, or if you’re in a warm or cold climate.
- Test for ketones with ketone sticks, which you should always bring with you on a trip. When your blood sugar is over the 270 mark (15 in UK numbers), get ketone testing.
Whether you intend on making a switch from an insulin pump to injections or not, it’s always a good idea to carry insulin pens with you when traveling. There are so many reasons that your pump could simply die. Especially if the climate conditions of the country you are visiting are extreme.
It’s important to know what to do and how to make the switch back to insulin pens when these situations arise. I hope you’ve found this information useful!
I’d love to know: have you ever made a short or long-term switch from an insulin pump to injections when traveling? Comment below and let me know!
If you would like a full-throttle guide packed with tips, resources, stories and more, then check out the e-book, The Ultimate Guide to Travelling with Type 1 Diabetes. You can get 40% off with the code BLONDE40.
Disclaimer: I am not a medical professional and all my words are based on my own personal travel experience and advice. I don’t take any responsibility for any problems or issues with type one diabetes. Please contact your diabetic nurse or doctor before embarking on a new journey! Happy travels!












It will help travellers much if they are travelling with diabetes. Thank you so much for sharing this post.
Nice guide lines about travel. I m also a traveler person.